More than 300,000 women in North Carolina aged 18 to 44 live in an area that does not have enough hospitals or birth centers – or in some cases, none at all. It is according to data from Ten Sous Marche.
UNC-Chapel Hill researchers use AI technology to provide more resources for mothers’ expectations.
“There are many places in North Carolina which do not have adequate access to ultrasounds,” said Dr. Jeffrey Stringer. “It is very difficult to provide obstetric care without ultrasound.”
Stringer is a teacher of obstetrics and gynecology at the UNC School of Medicine. He and his wife, who also work in the field, first noticed a need while working in Zambia for eleven years. Quick advance until 2025, and Strnger hopes to obtain technology in clinics and hospitals by the end of the year.
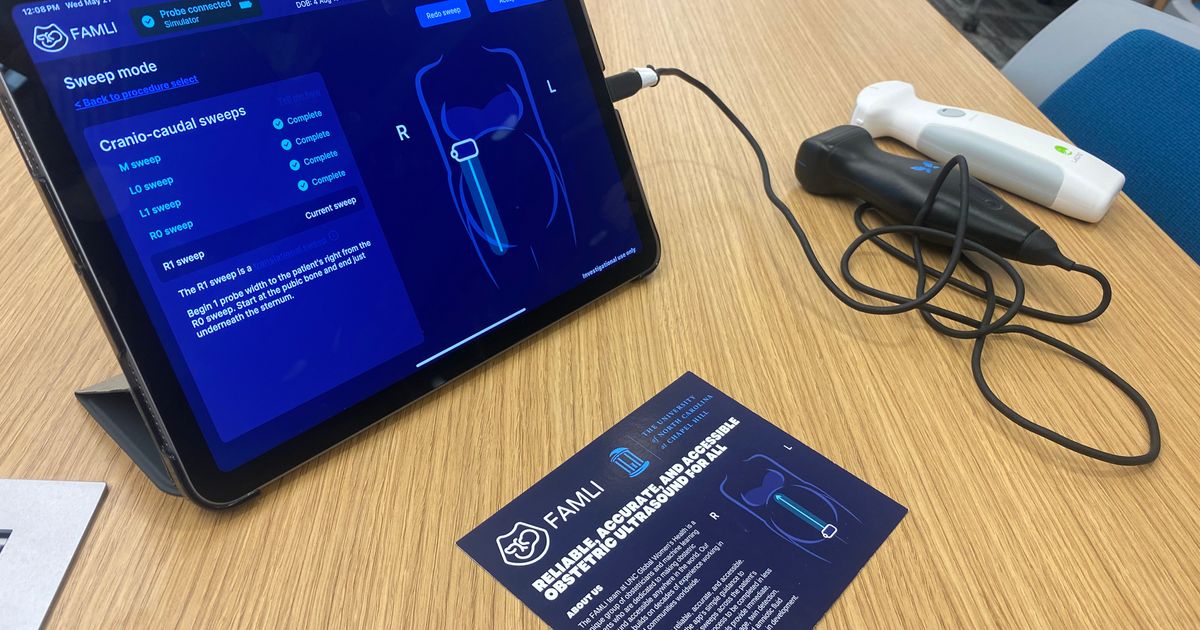
The Srihari Chari research project manager has helped develop the Famli application. Users connect ultrasonic devices powered by battery in a smartphone or tablet. The application then guides the user through ultrasound to collect data, including the age, size and position of the baby.
“On the screen screen, if there is something that could be worrying, we include a small yellow exclamation mark,” said Chari. “It is not supposed to be alarming for the patient. It’s just to say: “Hey, this patient may need additional care. »»
Strunger said the goal is to be able to increase its capacities to diagnose more in the future, such as certain congenital malformations or extrautterin pregnancies, which endanger life.
“The functions that we have integrated into the application at the moment are probably not enough to replace all the ultrasounds that take place in the remote counties in North Carolina,” he said.
Wral has asked for how precise AI results were so far.
“The AI is actually more precise than an expert suburb, using one of these most expensive machines … We know that clinical trials we have done,” replied Strunger. “It is wrong, sometimes. This is why we continue to work with technology to try to improve it continuously and to build in warm -up … It is an evolving technology.”
Stringer said the product is the result of more than 7 years of research and $ 20 million from various subsidies.
Wral previously reported earlier this month
“I am not saying to what to do. I collect tons of information, and I say:” Here are some examples “… and AI, itself, learns to distinguish these … To do it, you need gigantic amounts of data,” said Stringer. “By far, the most expensive aspect … is to collect this type of data.”
Currently, the application is only used for research purposes. However, the team has several applications to obtain the approval of the US Food and Drug Administration. Firstly, Stringer hopes to make the technology available in a medical environment, in particular in more rural counties that do not have obstetricians or obstetric care.
“Some women have high -risk pregnancies that should be monitored frequently,” said Stringer. “We are trying to do is to build AI tools that allow suppliers who have no formal ultrasound training to use them with competence.”
He finally wants people in the community to have access to technology, such as doubles or even the parents themselves.
“There is an idea that we are working on, that we are not so far, that is to say, is it possible for the patient himself to use it?” Said Strunger.
He said that the application was not intended to replace the medical staff, but instead, free them to respond to the more complicated cases.
“Our objective is not to replace the expert ultrasounder who makes these detailed anatomy analyzes … We are trying to build a simple tool that can be used at the lowest level of care as a screening modality which allows patients to obtain precise and precise results and to avoid having to drive 2 and a half hours,” he explained.
Not only would the application offer more accessibility to parents, but it would also help hospital systems save time and money on ultrasonic equipment.
“”[The app] Takes 2-3 minutes to collect data and produce diagnostics, “said Strnger.” It is very different than having an appointment and having to drive to obtain a normal ultrasound. »»
Wral noted that ultrasound -powered battery devices vary from $ 50 to $ 5,000. Full size machines that could be found in hospitals can cost up to $ 50,000, depending on Wral’s search.
Stringer and his team also test the product in developing countries, in the hope of also increasing accessibility – including Zambia.